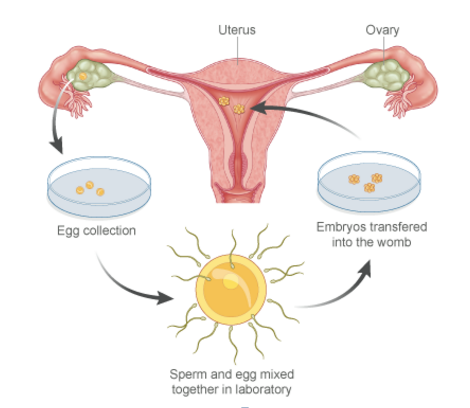
In-vitro fertilization is the process of fertilization where an egg is combined with a sperm under in vitro or laboratory conditions. This technique is a boon for all those childless couples who have failed to conceive and give birth to a baby through the natural process. IVF is especially beneficial in case of PCOS, blocked uterine tubes, fibroids, endometriosis, low ovarian reserve, and poor egg or sperm health. However, sometimes this procedure may not work out as planned and result in a failed IVF.
In Vitro Fertilization
Work From Home – A Ray of Hope for Patients seeking IVF Treatment
The demand for IVF treatment is gathering pace. This is because it has helped all those patients who were otherwise unable to conceive. The ultimate objective of IVF is to have a successful pregnancy and a healthy baby. However, today’s digitally driven and stressful corporate world has created a challenge for women who are looking to welcome Motherhood with the help of IVF treatment. However now there is a ray of hope as Work from Home is the new norm for most of the employees due to the current crisis caused by the pandemic.
Fertility Care – It’s all about being in Good Hands
Life presents us with many choices. It’s the choices we make that determine our future. This is all the more evident in the healthcare sector these days where patients would like to have multiple opinions before going ahead with the medical treatment advised by the physicians relevant to their specific health issues. In other words, patients would like to meet multiple doctors and take their individual opinions. This is also referred to as doctor shopping.
Brief History of IVF
Let’s start at the beginning. In-Vitro Fertilisation, or now more commonly known as IVF treatment saw a flicker of hope as early as the mid-1800s. In the mid-1800s, scientists finally discovered the process of artificial fertilization using a combination of sperm and egg.
Tube Reversal vs IVF Treatment : Which is the better Choice?
Attaining Motherhood and having children is one of the very important stages in life which a woman comes across. Though Pregnancy and Childbirth can get challenging at times, it is looked forward to as stage of immense significance, by every woman. While on one hand, birth control has become a topic for global discussion, on the other hand, there are many enthusiastic women, in their middle ages, who are looking at exploring options to extend their family, even after undergoing procedures towards achieving permanent birth control.
Misconceptions about IVF
IVF is one of the most fascinating discoveries of the 20th century. Nobel prize in medicine was awarded to Sir Robert G Edwards in 2010 for this amazing discovery. It has been about 40 years since the birth of the first child through IVF. Over 4 million people owe their existence to IVF. Despite this, many people are not convinced by this concept.
Things To Know Before Opting For IVF
Once a couple decides to go ahead with IVF(In vitro fertilization), the next concern is the IVF success rate and to decide when to go for IVF treatment. As we all know IVF has its limitations and a variety of factors influence the outcome. Some of them are under our control and some of them are not.
What is the Sucess Rate of IVF?
The outcome of an IVF cycle depends on the quality of the embryo which in turn depends on the egg quality and the sperm quality. Egg quality is mainly dependent on the age of the woman. As age increases, particularly in the late thirties, the chances of having aneuploid/ abnormal eggs increases.
ICSI( intracytoplasmic sperm injection) can overcome most of the sperm-related problems but severely abnormal semen samples can give rise to poor quality embryos, thereby compromising the IVF success rates. Egg numbers are equally important. Studies show that IVF success increases as the number of eggs retrieved increases up to about 15 eggs. Thereafter there is no further increase in the success.
Does the collection of eggs increase the chance of pregnancy from IVF?
The process of IVF(In-Vitro-Fertilization) involves the ovarian stimulation with hormones with the intention of retrieving more eggs. The whole idea is to have enough eggs to produce an optimum number of good embryos to transfer and to freeze a few in case the fresh transfer fails. The question here is how many do we actually need? What is the optimum number of eggs needed to achieve a live birth, which in turn is the ultimate aim of IVF?